Abstract
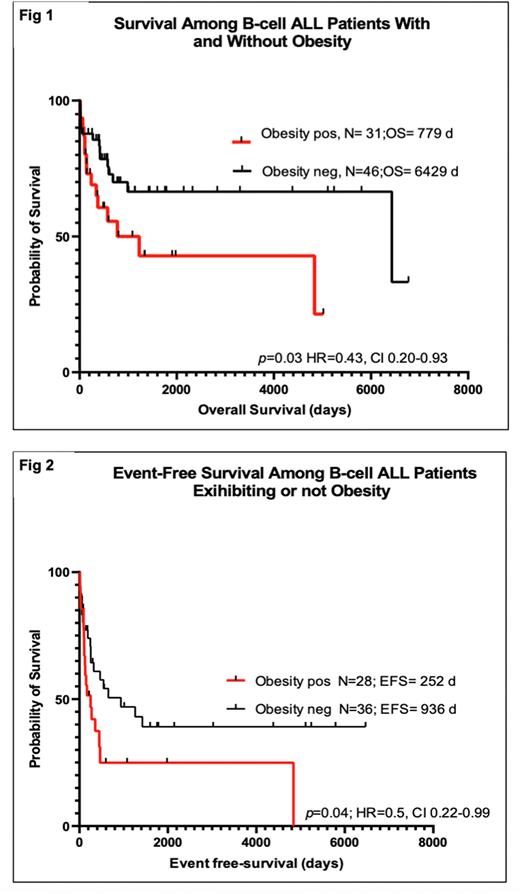
Background: Previously, obesity has been associated with increased risk of relapse in aggressive lymphoproliferative disorders [Teegaparavu. ASH.2021]. The mechanism is largely unknown. However, attenuated chemosensitivity driven by unbalanced adiponectin/leptin regulation and obesity specific tumor microenvironment defects represent interesting "reversible” factors. Additionally, it is possible that B-cells aberrantly proliferate under obesity induced cytokine/chemokine influence. In pediatric patients (pt), obesity correlates with suboptimal Measurable Residual Disease (MRD) after induction. High insulin levels and PI3K/ATK/mTOR activation render anti-apoptotosis and chemorefractoriness [Bresin. Cell Death & Disease. 2016]. In this study, we investigate the effect of obesity on overall survival (OS) and event free survival (EFS) in a cohort of adult B-cell Acute Lymphoblastic Leukemia (B-cell ALL) older than 40 years with and without pre-treatment obesity. Methods: After IRB approval, B-cell ALL patients (pt) treated under standard induction protocols were selected at the Instituto de Cancerologia in Mexico and Baylor College of Medicine Institutions from 2010 to 2019. Obesity was diagnosed according to standard definitions based on body mass index (BMI) to include class I, II and III subgroups (BMI>30). Detectable modification in OS and EFS were estimated by using the Kaplan Meier Method. Descriptive statistics summarized results. To assess the independent effect of intervening variables on outcomes of interest, cox regression model was performed. SAS software was used for analysis. Results: 46/71(64.7%) and 31/71 (43.6%) pt exhibited or not obesity. Median age for obese and not obese pt was 52 years (y) vs 56 y, respectively. WBC, LDH and blast at disease onset were 43.2 K/UL v 20.1 K/UL, p=0.02; 1009 U/L v 600 U/L, p= 0.2; 62.8% v 60.6% for obese vs not obese pt, respectively. Incidence of high risk genomic did not statistically differ when accounting for t (9; 22), hypodyploid karyotype, P53 and 11q23 abnormalities. OS was 779 days (d) v 6429 d, in pt with and without obesity, p=0.03 [HR=0.43, CI 0.2-0.93] [Fig 1]. When considered relapse risk, EFS was 252 d v 936 d, in pt with and without obesity, respectively, p= 0.04 [HR=0.50, CI 0.22-0.99] [Fig 2]. Univariate analysis revealed that high BMI [p=0.001] and higher WBC [p=0.04] were predictor for OS and EFS. Cox regression model demonstrated that high WBC independently predicted inferior OS and EFS, p=0.002, each. Conclusions: Obesity is associated with inferior OS and EFS in adult non- AYA pt diagnosed with B-cell ALL. High BMI >30 is associated with enhance risk of relapse, which may explain, at least in part inferior OS in our pt cohort. Higher WBC at disease onset suggests that obesity is linked with blast proliferation efficiency. Deeper understanding of obesity induced metabolic abnormalities leading to B-cell ALL chemorefractoriness is needed. Weight reduction via caloric restriction and exercise may represent interesting interventions to improve clinical outcome of leukemic pt with high BMI.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal